Celiac disease, an autoimmune disorder triggered by gluten, poses significant dietary restrictions for those affected, impacting not just food choices but also the consumption of beverages like whiskey. Originating from grains that contain gluten, whiskey’s compatibility with a gluten-free lifestyle hinges on its distillation process, which theoretically removes gluten proteins. This exploration seeks to dissect the intricate dynamics between celiac disease and whiskey consumption, providing essential insights for individuals striving to adhere to a gluten-free diet while contemplating the safety and enjoyment of whiskey. Through a detailed examination of celiac disease’s symptoms, diagnosis, and treatment, alongside the gluten content in whiskey, this article aims to equip readers with the knowledge to make informed decisions regarding whiskey consumption in the context of celiac disease, addressing prevailing medical perspectives and individual tolerance considerations.
What is celiac disease?
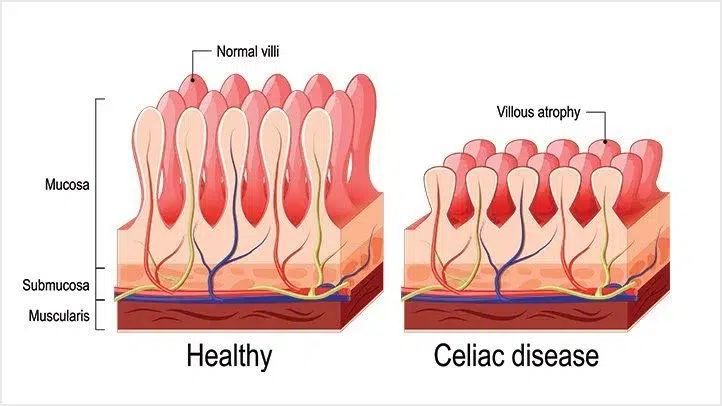
Celiac disease is an autoimmune condition characterized by the body’s adverse reaction to gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system responds by attacking the small intestine, leading to inflammation and damage to the villi, the tiny fingerlike projections lining the intestine. This damage impairs the body’s ability to absorb nutrients effectively, resulting in a range of digestive and non-digestive symptoms.
The condition is driven by a combination of genetic predisposition and environmental factors, making it necessary for those diagnosed to follow a strict gluten-free diet. This dietary adjustment is the cornerstone of managing celiac disease, as it helps to mitigate symptoms and promote intestinal healing.
Diagnosis of celiac disease typically involves two critical steps: conducting blood tests for specific antibodies indicative of an autoimmune response to gluten, and performing an endoscopic biopsy of the small intestine to directly observe the extent of villous atrophy and inflammation.
How is celiac disease diagnosed?
The diagnosis of celiac disease hinges on a two-step approach that begins with blood tests. These tests search for specific antibodies that are elevated in individuals with celiac disease, acting as markers for an autoimmune reaction against gluten. Elevated levels of these antibodies suggest an immune response that is characteristic of celiac disease.
If the blood tests indicate potential celiac disease, the next step involves an endoscopic biopsy of the small intestine. This procedure allows healthcare professionals to take a closer look at the intestinal lining for damage or inflammation, particularly the flattening of the villi. The villi are essential for nutrient absorption, and their damage is a hallmark of celiac disease.
Together, the combination of blood tests and an endoscopic biopsy forms a comprehensive diagnostic framework, ensuring an accurate diagnosis and laying the groundwork for effective management and treatment of celiac disease.
Blood tests for specific antibodies
The diagnostic journey for celiac disease often begins with blood tests aimed at identifying specific antibodies. These antibodies, notably anti-tissue transglutaminase (tTG) and anti-endomysium (EMA), become elevated in response to gluten in individuals with celiac disease. Elevated levels suggest an autoimmune reaction to gluten, serving as a preliminary indicator of the condition. These tests are essential for pinpointing candidates who may benefit from further diagnostic scrutiny through an endoscopic biopsy.
Endoscopic biopsy of the small intestine
Should blood tests reveal elevated antibody levels, an endoscopic biopsy of the small intestine is the next critical step. This procedure entails collecting tissue samples from the small intestine’s lining, which are then meticulously examined for signs of villous atrophy—the hallmark damage observed in celiac disease. The presence of such damage under microscopic analysis confirms the diagnosis of celiac disease, providing a clear direction for subsequent treatment and management strategies.
What are the symptoms of celiac disease?
Celiac disease presents a complex spectrum of symptoms, which can vary widely among affected individuals. Digestive symptoms are prevalent, especially in adults and children, and include issues such as abdominal pain, bloating, diarrhea, and constipation. These symptoms often lead to the initial suspicion of celiac disease.
Beyond the digestive tract, celiac disease can manifest through a variety of non-digestive symptoms. These may include anemia, fatigue, bone or joint pain, and skin rashes like dermatitis herpetiformis, underscoring the systemic impact of the disease. The diversity and overlap of symptoms with other conditions make celiac disease a challenging puzzle for both patients and healthcare providers.
Understanding the broad range of potential symptoms is critical for achieving a timely and accurate diagnosis. This knowledge empowers individuals to seek appropriate testing and treatment, primarily a gluten-free diet, which is the cornerstone of managing celiac disease and mitigating its symptoms.
Digestive symptoms in adults and children
Celiac disease primarily reveals itself through a suite of digestive symptoms that affect both adults and children. These symptoms include abdominal pain, bloating, diarrhea, and constipation. The root of these issues lies in the immune system’s response to gluten, which damages the lining of the small intestine, impairing its ability to absorb nutrients effectively. Early recognition and management of these symptoms are pivotal, guiding individuals towards necessary dietary adjustments to alleviate discomfort and promote healing.
Non-digestive symptoms that may occur
Beyond the digestive tract, celiac disease can manifest through a range of non-digestive symptoms, illustrating the condition’s systemic impact. Individuals may experience anemia, a result of compromised nutrient absorption, fatigue, bone or joint pain, signaling deficiencies in calcium and vitamin D, and skin rashes, such as dermatitis herpetiformis, a direct consequence of gluten ingestion. These varied symptoms underscore the importance of a holistic approach to diagnosis and management, emphasizing the need for a gluten-free diet to mitigate the wide-ranging effects of celiac disease on the body.
What is the cause of celiac disease?
The onset of celiac disease is attributed to a combination of genetic predisposition and environmental factors, with gluten serving as the primary environmental trigger. Individuals carrying certain genetic markers are more susceptible to developing the condition. However, the presence of these markers alone does not guarantee the disease’s manifestation, underscoring the significant role environmental factors play.
Gluten, a protein found in wheat, barley, and rye, triggers an autoimmune response in those predisposed to celiac disease. This response leads to inflammation and damage within the small intestine, notably affecting the villi responsible for nutrient absorption. The resulting malabsorption can cause a wide array of symptoms and contribute to long-term health complications if left untreated.
Understanding the root causes of celiac disease is crucial for effective management, primarily through the adherence to a strict gluten-free diet. This approach not only alleviates symptoms but also promotes intestinal healing, highlighting the importance of recognizing and addressing both genetic and environmental factors in the treatment of celiac disease.
Genetic predisposition and environmental factors
At the heart of celiac disease lies a genetic predisposition, with certain genes significantly elevating the risk of developing the condition. Yet, the genetic aspect is only part of the equation; environmental factors are equally critical. The interplay between genetic susceptibility and environmental triggers, particularly the consumption of gluten, is key to the onset of celiac disease. This dual influence underscores the necessity for a comprehensive approach in understanding, managing, and potentially preventing the disease by considering both genetic and environmental aspects.
The role of gluten in triggering symptoms
Central to the development of celiac disease symptoms is gluten, a protein found in common grains such as wheat, barley, and rye. In individuals with celiac disease, ingesting gluten leads to an autoimmune response, characterized by inflammation and subsequent damage to the lining of the small intestine. This autoimmune attack compromises the intestine’s ability to efficiently absorb nutrients, culminating in the wide array of symptoms associated with the condition. Acknowledging gluten’s critical role in symptom manifestation is pivotal, highlighting the importance of a strict gluten-free diet as the cornerstone of effective celiac disease management.
How is celiac disease treated?
Treating celiac disease revolves around a strict adherence to a gluten-free diet, the cornerstone of management for this condition. Eliminating gluten from the diet is essential, as it halts the immune response and inflammation, allowing the small intestine’s lining to heal. Over time, this dietary adjustment can lead to a significant improvement in nutrient absorption and a reduction in symptoms, enhancing the quality of life for those affected.
In addition to dietary changes, nutritional supplements may be necessary to address potential deficiencies in vitamins and minerals resulting from the malabsorption issues associated with celiac disease. Supplements can help restore nutritional balance, supporting overall health and recovery.
Effective management of celiac disease requires a lifelong commitment to a gluten-free lifestyle, underscored by regular medical consultations. These follow-ups ensure the disease is adequately monitored and that the dietary regimen continues to be effective in managing the condition.
Strict adherence to a gluten-free diet
Central to the treatment of celiac disease is strict adherence to a gluten-free diet. This regimen involves eliminating all foods containing gluten, which is found in wheat, barley, and rye. The exclusion of gluten from the diet is imperative to cease the autoimmune response and inflammation damaging the small intestine. Adopting a gluten-free lifestyle allows the intestinal lining to recover, fostering an environment where nutrient absorption is optimized. This dietary commitment is vital for alleviating symptoms, promoting healing, and ensuring a return to health for those diagnosed with celiac disease.
Nutritional supplements to address deficiencies
Given the malabsorption issues inherent in celiac disease, nutritional supplements are often necessary to rectify deficiencies in essential vitamins and minerals. Supplementation with iron, calcium, vitamin D, and various B vitamins can be crucial for replenishing depleted nutrient stores. These supplements are especially important during the initial phase of adopting a gluten-free diet, aiding in the correction of nutritional imbalances and supporting the healing process of the intestinal lining. Tailored supplementation, guided by healthcare professionals, ensures that the specific nutritional needs of each individual are met, laying the foundation for effective disease management and recovery.
What is gluten?
Gluten is a complex protein found predominantly in wheat, barley, and rye. It gives bread its elasticity and chewiness and acts as a binding agent in many other food products. For those with celiac disease, however, gluten acts as a trigger for an autoimmune response that leads to the damage of the small intestine’s lining. Recognizing the sources and understanding the impact of gluten is essential for anyone needing to manage gluten-related disorders. A strict gluten-free diet becomes necessary to mitigate symptoms and facilitate the healing of the intestine, highlighting the importance of gluten awareness in dietary choices.
Found in wheat, barley, and rye
Gluten, the protein implicated in celiac disease, resides chiefly in wheat, barley, and rye. These grains form the foundation of numerous food products, including bread, pasta, and beer, as well as being components in various sauces and processed foods. For those diagnosed with celiac disease or exhibiting gluten sensitivity, recognizing and avoiding these grains is essential. This knowledge is foundational for maintaining a gluten-free diet, crucial for preventing the autoimmune response and promoting intestinal health.
Does whiskey contain gluten?
Whiskey, traditionally distilled from gluten-containing grains such as wheat, barley, and rye, enters a complex debate regarding its gluten content. The distillation process, which whiskey undergoes, theoretically removes gluten proteins, suggesting that distilled spirits might be safe for individuals with celiac disease or gluten sensitivity. However, this assertion hinges on the efficiency of the distillation process and the absence of gluten cross-contamination post-distillation. As such, whiskey’s status as a gluten-free beverage remains a topic of discussion among those maintaining a gluten-free diet, highlighting the need for careful consideration and, often, personal discretion.
The distillation process theoretically removes gluten
Central to the production of whiskey is the distillation process, which theoretically removes gluten from the beverage. This process involves heating the liquid until it vaporizes, with the vapor then being cooled to condense back into liquid form. Gluten proteins, due to their inability to vaporize at the temperatures used in distillation, are theoretically left behind in this process. This foundational principle supports the assertion that whiskey, even when derived from gluten-containing grains, could be deemed safe for consumption by individuals with gluten sensitivities or celiac disease, contingent upon the effectiveness of the distillation process and absence of post-distillation gluten contamination.
Can people with celiac disease safely consume whiskey?
The safety of whiskey consumption for individuals with celiac disease is a matter of ongoing debate among medical professionals. While the distillation process theoretically removes gluten proteins, making whiskey potentially safe for those with gluten sensitivities, concerns about cross-contamination and trace gluten levels warrant caution. The reality is that individual tolerance levels may vary; some people with celiac disease may enjoy whiskey without experiencing any adverse effects, whereas others could encounter symptomatic reactions. Given these variables, it is crucial for those with celiac disease to seek personalized advice from healthcare providers before deciding to include whiskey in their diet, ensuring an informed and health-conscious decision is made.
The ongoing debate among medical professionals
At the heart of the discussion on whiskey consumption for individuals with celiac disease is an ongoing debate among medical professionals. Divergent views exist, with some experts suggesting that the distillation process effectively eliminates gluten, rendering whiskey safe for those with gluten sensitivities. Conversely, others raise concerns about the potential for cross-contamination and the presence of trace gluten amounts, advocating for caution. This debate highlights the need for continued research and clearer guidelines to navigate the complexities of diet management in celiac disease.
Individual tolerance levels may vary
A critical consideration in this debate is the acknowledgment that individual tolerance levels may vary significantly among those with celiac disease. While some may enjoy whiskey without adverse reactions, others could experience symptoms due to trace gluten exposure. This variability underscores the importance of a personalized approach to managing celiac disease. It emphasizes the necessity for individuals to closely monitor their own responses and seek personalized advice from healthcare professionals before incorporating whiskey into their diet, ensuring decisions are informed and tailored to their specific health needs.
What are the considerations for people with celiac disease when consuming whiskey?
For individuals with celiac disease, navigating whiskey consumption requires careful consideration. Initially, it’s essential to understand the labeling and regulations related to gluten in alcoholic beverages, which can provide valuable guidance. However, the challenge is compounded by the lack of standardized gluten-free labeling for spirits, including whiskey, making it difficult to make informed decisions.
Given the ongoing debate among medical professionals regarding the safety of distilled spirits, individuals must also reflect on their individual tolerance levels to gluten, which can vary significantly. For those seeking additional reassurance, opting for certified gluten-free products offers a safer alternative.
Lastly, the importance of consulting healthcare providers cannot be overstated. Personalized advice from medical professionals can help those with celiac disease make informed decisions about including whiskey in their diet, ensuring their health and well-being are prioritized.
Labeling and regulations regarding gluten in alcoholic beverages
Understanding the labeling and regulations pertaining to gluten in alcoholic beverages is essential for those with celiac disease. Regulatory standards can vary widely, making it crucial for individuals to familiarize themselves with the guidelines that govern gluten content declarations on alcoholic products, including whiskey. This knowledge aids in making informed and safer consumption choices.
The lack of standardized gluten-free labeling for spirits
A notable obstacle is the lack of standardized gluten-free labeling for spirits. This inconsistency across the industry complicates the ability of individuals with celiac disease to identify safe products confidently. Advocacy for uniform gluten-free labeling standards is vital to address this challenge and enhance product transparency.
Recommendations for those with celiac disease consuming whiskey
For those with celiac disease, recommendations generally advise caution regarding whiskey consumption. Considering the potential risks, including gluten cross-contamination and sensitivity to trace amounts, prioritizing health by carefully evaluating the decision to consume whiskey is recommended.
Opting for certified gluten-free products when available
Seeking out certified gluten-free products offers a safer alternative for individuals with celiac disease. These products have been rigorously tested to meet established gluten-free criteria, providing a higher degree of assurance regarding their safety and suitability for a gluten-free diet.